How current physical therapists became diagnosticians illuminates the trajectory of the profession and the value we offer. My recent exploration into this American story was recently published as an historical essay in Physical Therapy & Rehabilitation Journal (PTJ). Here, I provide a brief overview of the article.
Transformation didn’t occur suddenly. It happened over a period of decades, with a number of factors converging around the same time. Below are some of the key factors in the journey:
Strong Friends
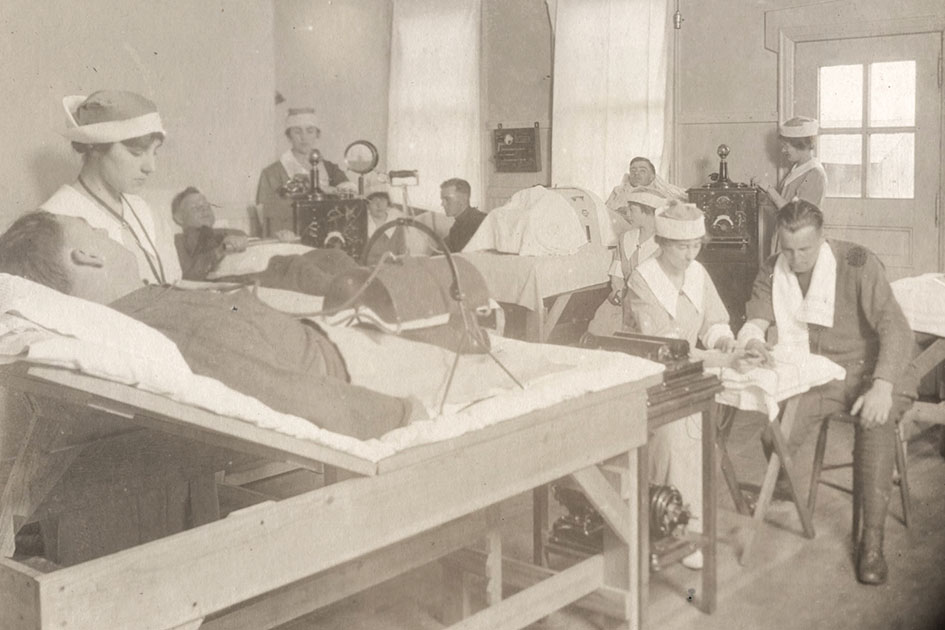
In the US, Reconstruction Aides were formed in World War I to assist “physical therapy physicians” provide treatment to their patients. Post war, the formation of a member association – now the American Physical Therapy Association (APTA) – and other actions attempted to strengthen the profession in the hopes that it would continue. Another strategy of early physical therapists was to align themselves very closely with physicians; almost obsequiously. They wanted no confusion about one fact: physical therapists did NOT render diagnoses. Evidence of this is seen in the first Code of Ethics, in which the first point clearly prohibits diagnosis by a physical therapist.
Neurological Rehabilitation
Following World War II, with uncontrolled hypertension, cars without seatbelts and polio ongoing, there was a swell of patients with neurological conditions who befuddled physicians. Howard Rusk, recognized as one of the early “physiatrists” (who evolved from the physical therapy physicians) stated in his autobiography that he would deliberately avoid these patients, as he knew no way of helping them. As a result, physical therapists at the time were largely left to experiment with treatments that might be of some benefit. While not necessarily diagnosing, they began to assume greater responsibility for patient care and honed their observational skills. A testament to this was the international popularity of Proprioceptive Neuromuscular Facilitation, developed by a physician and physical therapist (Henry Kabat and Maggie Knott, respectively) together.
Manual Therapy
Although manual therapy was being taught earlier, there was an explosion in manual therapy education around this time. Probably the most relevant here is James Cyriax’s “selective tissue tensioning.” By teaching physical therapists how to go through what was essentially a framework for recognizing aggravated structures, James Cyriax (a physician) was giving tacit approval for his pupils to diagnose musculoskeletal conditions on their own. Others, like James Mennell, would urge physical therapists to move into this arena. It is also notable that as imaging developed, physicians put less emphasis on the physical examination. This left a gap for physical therapists to fill by becoming the providers that could perform more detailed physical examinations.
State Licensure
Physicians originally controlled licensure of physical therapists. As this changed, physical therapists began to control their own destiny, making their own rule. This was strengthened as physical therapists later developed their own accrediting association to control their education.
Health Insurance
It is astounding to reflect on how rapidly health insurance became the main way to pay for healthcare in the US. At the beginning of the 20th century, physicians basically bartered with patients and used a sliding scale for payment. By 1970, the vast majority of healthcare was paid for with insurance. This was important, particularly later, as battles over direct access, etc., centered around rules established by insurance companies and not necessarily state law. Private practices also began to expand around this time in physical therapy. Physically remote from physicians, it became simpler for PTs to modify treatment and render diagnoses independently.
Recognition of Expertise
There are many instances of physicians promoting the expansion of scope by physical therapists. This was also the case in the US Army, where two physicians successfully used physical therapists as “screeners” for patients with low back pain. Their study was published in Physical Therapy Journal in 1975, and is likely the origin of physical therapists discussing “screening” for red flags in low back pain, a term that was coined years earlier but rarely used by physical therapists. Around the same time, physical therapists were already seeing themselves as specialists in certain areas, and the APTA began to explore the possibility of developing those specialties.
Internal Discussion About Diagnostic Frameworks
Once the APTA formally recognized the ability of physical therapists to render diagnoses, a flurry of papers were published in which physical therapists debated the best methods. Perhaps because of their continued unwillingness to infringe on the scope of physicians, or perhaps recognizing the failure of pathoanatomic diagnoses, a lot of the discussion focused on “classification” approaches. These debates still continue today, although the APTA has adopted the International Classification of Functioning, Disability and Health (ICF) model in their documents. The APTA is also looking into the potential of movement diagnoses, which would theoretically fit within the ICF model and identify impairments of the proposed “movement system.”
Conclusion
There are two big lessons from reviewing the history of physical therapists and diagnosis in the US. First, change takes time. It’s worth noting that even after the APTA officially recognized the ability of PTs to diagnose, some physical therapists had their licenses suspended for doing so because it wasn’t allowed in their state. Second, that practice often initiates change. If you notice, the APTA was almost never the one to initiate change, it responded to it. By the time the APTA recognized the ability of PTs to diagnose, research showed they already had been doing it for some time.
References
Petersen S. 2023. How Physical Therapists became Diagnosticians: An American History. Physical Therapy & Rehabilitation Journal. Accessed online at https://academic.oup.com/ptj/advance-article/doi/10.1093/ptj/pzad049/7205198 on 13 July 2023.