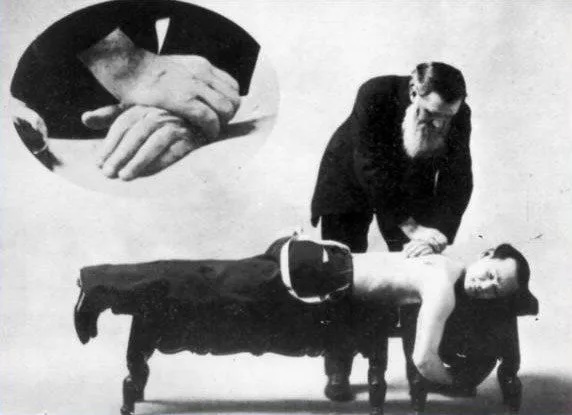
Osteopathy was devised in 1870s America by Dr Andrew Taylor Still (1828-1917) and chiropractic some twenty years later by David Daniel Palmer (1845-1913). Both utilised a structural perspective to explain and treat functional disturbances. Over the years, orthodox medicine viewed such practices with disdain. The wide variance in training, lack of scientific basis, and preference of some practitioners to behave in the manner of ‘snake-oil salesman’ did not endear them to the medical profession. However, the simple procedures, and the down-to-earth nature of many of the practitioners, saw them welcomed more warmly by those alienated by the perceived conceit, wealth, and incapacity – at least as far as effecting a cure was concerned – of some medical practitioners.
Both practices were introduced into Britain, and thereafter her dominions such as New Zealand and Australia, in the early years of the twentieth century. For the first half of the century numbers in both professions remained low but they were popular in rural areas. Country folk often led physical lifestyles more prone to sustaining musculoskeletal injuries and they reacted favourably to the no-nonsense style of many of the practitioners.
Manipulation of the joint, and especially the spinal vertebrae, had been a long-established folk therapy. It had been practised by bonesetters in the eighteenth and nineteenth centuries and had later been incorporated by Hugh Owen Thomas (1834-1891) into the foundations of modern orthopaedic practice. However, the association of manipulation with ‘fringe’ practitioners meant that it was suspect practice in the eyes of many medical doctors.
There were those, however, who felt that the dismissal of all manipulative techniques, on the basis of the dubious quality of some practitioners was ‘to throw the baby out with the bath water’. In particular, Dr James Mennell (1880-1957), of St Thomas’ Hospital in London, spent his career seeking to demonstrate that there was a place for manipulation in the armoury of any medically trained physiotherapist. Mennell’s work was continued at St Thomas’ by Dr James Cyriax (1904-1985), who considered that the demand for the therapy was going to always exist, so it was better if it was performed by a therapist fully trained in anatomy, pathology and movement, and who was part of the orthodox medical system.
Both Mennell and Cyriax influenced the early practice of spinal manual therapy by Australian physiotherapists. This came through their books, and in the case of Cyriax, personal contact, both with Australians visiting St Thomas’ and as a visiting lecturer in Australia and New Zealand in the 1950s.
One of the champions of clinical manipulation in Australia was the orthopaedic surgeon at Melbourne’s Alfred Hospital, Dr Charles Hembrow (1898-1983). Due to his wisdom and courage, lecturers were given permission to teach physiotherapists the basic principles of manipulation in Victoria. Instruction was provided to male students only as a substitute for the regular instruction in antenatal care.
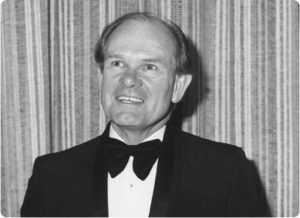
Geoffrey Maitland
The person who made the most significant contribution to the establishment of manipulative therapy in Australia was Geoffrey Maitland (1924-2010). Through study and observation Maitland became a world authority of the subject. His range of informants ran from physiotherapists and orthopaedic surgeons to osteopaths. As well, he quizzed his patients as to what chiropractic treatment worked for them. Maitland also travelled to the UK and the USA in the early 1960s, spending time with Dr Cyriax and physiotherapists Gregory Grieve and Jennifer Hickling, and at the London School of Osteopathy with Dr Allan Stoddard. Maitland’s form of assessment, with its focus on the identification of local soft-tissue or joint restriction as a source of dysfunction represented a substantial change for the profession, which had previously relied on massage, electricity and general exercises.
Manipulative therapy was found to give good results with back pain, one of the most prevalent conditions physiotherapists had to deal with. In the eyes of many practitioners, it was simpler and cheaper approach than the use of drugs or surgery. Australian physiotherapists enthusiastically adopted Maitland’s techniques and special interest groups were formed where practitioners could meet and exchange information. Over time Maitland’s approach was instrumental in gaining the tacit approval of the medical profession for the practice of manipulation.
One unintended consequence of medical acceptance of manipulation was the increased popularity of chiropractic and osteopathy. Following the Second World War, chiropractors and osteopaths had begun to increase in number and seek legitimation. Chiropractic was the most militant, and from its beginnings the practice had defined itself by its opposition to the medical establishment, thereby attracting publicity and support. Certain members of Parliament were suspicious of the perceived privilege of the medical establishment, while others were ‘believers’ who had first or second-hand experience of the apparent efficacy of the practices involved.
From the 1960s onwards chiropractic and osteopathy began to lobby harder for greater recognition. They met with politicians, held public meetings and endeavoured to mobilise public support. Their efforts eventually bore fruit and they were included in a number of State and Federal government inquiries into the field of ‘alternative medicine’. The Australian Physiotherapy Association (APA), along with the Australian Medical Association (AMA), made submissions to all of these committees advising against any form of official recognition.
The medical lobby considered the foundations of chiropractic and osteopathy to be scientifically unsound. Further, their standard of training was seen as inadequate for dealing with many medical conditions. On top of these wider concerns the physiotherapy profession also had some that were ‘closer to home’. Whilst the ethical requirements that physiotherapists treat patients only with a doctor’s referral had forged close links between physiotherapy and the wider medical profession, it did have its drawbacks. For example, chiropractors and osteopaths by being ‘free agents’ could see patients without referral. In a 1976 interview on Queensland radio, the then president of the Australian Chiropractors Association, Malcolm Rutledge, goaded physiotherapists claiming,
The physiotherapist is basically a second-string practitioner. He is not a first contact practitioner, he doesn’t directly contact the patient, he must go through the medical profession and we feel that the physiotherapist could be used in a similar fashion by the chiropractor to provide massage and passive mobilisation for the patient”.
For all their power and influence the medical lobby was ultimately unsuccessful in curtailing the practice of chiropractic and osteopathy. By the end of the 1970s, all Australian states had passed Registration Acts for their professions. In the public relations duel the orthodox medical authorities were outflanked. Convinced of the legitimacy of their point of view they were easily characterised as adopting a superior, almost arrogant tone. Chiropractors and osteopaths were able to present themselves as underdogs, aggrieved and even denigrated. The exclusionist approach taken by the medical establishment served to put many people off-side, regardless of their opinions of chiropractic or osteopathy. The appeal to the potential dangers of the practices provoked others to proclaim this as a reason to favour registration and thereby the imposition of minimum standards.
Inadvertently, the medical lobby did some of chiropractic’s work for it. In the mid-1960s a government-supported investigation by the Victorian branch of the AMA presented minimum criteria under which registration of chiropractic should be considered. This presented the Chiropractic Association with concrete goals to work towards, and ultimately led to the establishment of a training school, which was one of the principal requirements of the report.
As a consequence of chiropractic growth, physiotherapists began to look more closely at their profession in ways quite unthinkable fifty years previously. Through the creation of special interest groups and the incorporation of manual therapy in the physiotherapy education system, physiotherapy itself had grown. Graduates were better and more widely trained, and postgraduate research was being undertaken. Additionally, the move of the profession away from being located primarily in hospitals and into the wider community had seen physiotherapists become more involved in preventive medicine, which, ideally, required the ability to initiate treatment.
A significant body of knowledge on human movement was now being compiled within the profession. Physiotherapists, therefore, were often in a better position than many doctors when it came to diagnosing and prescribing treatment for musculoskeletal ailments. Yet, the need for medical referral was a frequently-used weapon by the chiropractic profession to diminish the importance of physiotherapy by noting that they were not independent practitioners. Operating only on medical referral began to be questioned, leading the profession in taking greater strides for independence in the 1970s.
In response the APA chose to repeal their first ethical principle, which stated that physiotherapists would only treat patients referred to them by a registered medical or dental practitioner. This was a change not taken lightly, for it was a founding principal of the profession as a way of demonstrating their belief in the efficacy of medical science and a means of gaining legitimacy through medical alliance.
The removal of the APA first ethical principle was a major step within Australia, and it caused waves on the world stage. Some countries, such as the UK had debated the issue but Australia was the first to actually enact the change. Not all nations were comfortable with the move, seeing a subordinate role to the medical profession advisable. Through lobbying and convincing oratory, the Australians succeeded in their mission at the 8th World Confederation of Physical Therapy (now World Physiotherapy) General Congress held in Israel in 1978.
Ultimately the move to primary contact status raised the standard and status of the physiotherapy profession. Greater responsibility helped the profession mature, and this in turn garnered greater respect from other branches of medicine and the wider community. A physiotherapist’s opinion began to be given more credence both clinically and administratively, with more invitations forthcoming to sit on planning and consultative committees. Public awareness of the profession was also raised by physiotherapists now being able to treat acute conditions more promptly.
References:
Bentley, PG. (2006). The Path to Professionalism: Physiotherapy in Australia to the 1980s. Australian Physiotherapy Association: Melbourne.

Great article Glenn, thanks for the share