The introduction of General Management into the National Health Service (NHS) in the United Kingdom (UK) which commenced in 1983/1984 was one of the most extensive and radical sets of changes to have taken place in the Service during its 73-year history. Arguably, the Griffiths recommendations which brought general management into the NHS set the scene for many further radical changes which have taken place since that time, and the history of the introduction of general management echoes through the succeeding decades in many ways. The Chartered Society of Physiotherapy (CSP) document – a primary source – at the end of this brief introduction to the topic sets out an overview of what was feared as possible detrimental outcomes for physiotherapy and healthcare provision as a whole, together with proposing best solutions for the leadership and management of physiotherapy services in the UK.
General management was introduced into the UK National Health Service (NHS) following the publication of the “National Health Service Management Inquiry”, Griffiths Report (Griffiths, 1983), and the subsequent Department of Health and Social Security (DHSS) Circular HC(84)13 and “Health Services Management Inquiry Implementation of the NHS Management Inquiry Report (DHSS, 1984).
The UK Government’s decision to implement general management throughout the NHS meant that health authorities were required to bring about changes in their management structures. To comply with this policy it was necessary for health authorities to review all of their management arrangements including the organisation and management of clinical services such as physiotherapy.
The NHS Management Inquiry
For several years the Government led by Prime Minister Margaret Thatcher had been dissatisfied with what they argued was ineffective and inefficient Consensus management across all sectors of the NHS.
In the House of Commons on the 3rd February 1983, Mrs. Jill Knight MP asked the Secretary of State for Social Services, The Rt. Hon. Norman Fowler, if he will make a statement on his plans to control manpower in the NHS (Hansard, 1983). Mr. Fowler’s reply to this written question was:
I have today established an independent NHS management inquiry into these matters. Health authorities in England have a revenue budget of almost nine billion pounds; employ about a million people; and spend almost seventy-five per cent of their revenue on pay. The Government needs to be satisfied that these considerable resources are managed efficiently and give the Nation value for money. The inquiry will be led by Mr. Roy Griffiths, Deputy Chairman and Managing Director of J. Sainsbury PLC.” (Hansard 1983).
Sir Roy Griffiths, in his letter attached to his report, stated, “We were asked by you in February to give advice on the effective use of manpower and related resources in the NHS; to inform you as our inquiries proceeded and to advise you on progress by the end of June”. (Griffiths 1983).
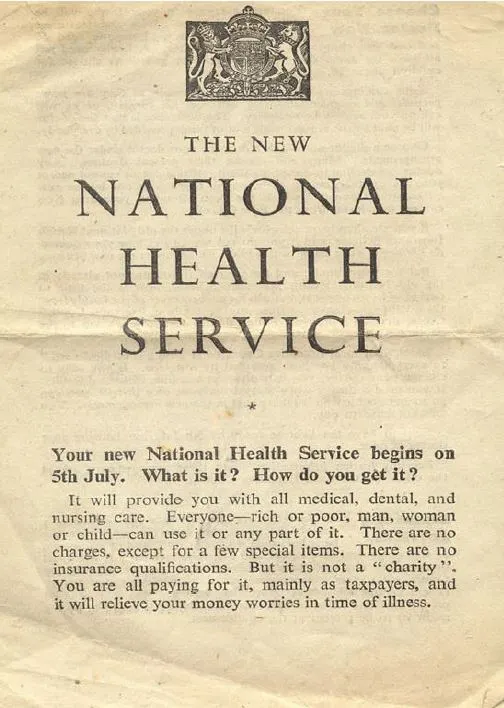
This seemingly straightforward and innocuous request by the Secretary of State was to prepare the way for the most radical and innovative series of changes in the management and organisational structure of the NHS that had taken place since its introduction in 1948.
Griffiths and the Inquiry Team
The Griffiths team was made up of members who were experienced in business management rather than health care. Sir Roy, Chairman of the inquiry team, was the Managing Director of the Sainsbury’s food chain; Michael Bett was Personnel Director of British Telecom; Jim Blyth, Head of Defence Sales at the Ministry of Defence and Sir Brian Bailey was Chairman of Television South West.
The inquiry philosophy and outcomes were clearly influenced by the business backgrounds of the team members. Griffiths observed:
We were brought in not to be instant experts in all aspect of the NHS, but because of our business experience and to advise on the management of the NHS. We have been told that the NHS is different from business in management terms, not least because the NHS is not concerned with the profit motive and must be judged by wider social standards which cannot be measured. These differences can be greatly overstated”. (Griffiths 1983)
The Griffiths Inquiry was unique in the history of official investigations into the management and working of the NHS. The inquiry team comprised only four members and there were no clinical interests represented in contradistinction to the many previous bodies which had reported to successive Secretaries of State on various aspects of the management of the NHS. The Report “Management arrangements for the reorganised NHS” – Grey Book (DHSS 1972) and the “Rehabilitation Report of a Sub-Committee of a Standing Medical Advisory Committee” (Tunbridge Report – DHSS 1972a) are just two examples of the plethora of Inquiries and Reports where the committees were very large (both having more than fifteen members) and a substantial number of the members were from the medical profession, nursing, other professions, and the DHSS. However, the membership of the Griffiths team was not the only feature that made the Griffiths Inquiry unique.
Findings and Style of the Griffiths Inquiry
Griffiths concluded that there was a lack of drive in the NHS because at each level of management there was no single person held accountable for action; decisions were delayed or avoided leading to an inefficient service. The Report stated:
It still lacks any real continuous evaluation of its performance…rarely are precise management objectives set; there is little management of health output; clinical evaluation of particular practices is by no means common and economic evaluation of those practices is extremely rare. One of our most immediate observations from a business background is a lack of a clearly defined general management function throughout the NHS. If Florence Nightingale were carrying her lamp through the corridors of the NHS today she would almost certainly be searching for the people in charge”. (Griffiths, 1983)
In summary, in the section of the Inquiry Report entitled “General Observations” Griffiths set out in detail what he considered to be the advantages of the general management process. In its advocacy of general management, the team was damning of functional management in that the advantages of the functional specialisms were offset by the need to establish the general management process effectively. Consensus management methods were vigorously criticised as being responsible for the making of “Lowest Common Denominator decisions” which he argued were weak and of poor quality. NHS management was thought by the Griffiths team to be reactive and passive rather than proactive and there was a lack of management data on “consumer” views. Much of the Report was about changes that the team thought were needed in attitude, understanding, and expectations as well as the style and method of management across the whole NHS.
As a result of the adoption of the Griffiths proposals by the Government, many wide-ranging and substantial changes in NHS organisation, management and leadership were implemented throughout the whole NHS starting in 1984 when the Government required that Health Authorities must “review in-depth their present management arrangements and to develop proposals to meet their own priorities and needs” (Annex “B” to Health Circular HC(84)13. The Griffiths recommendations were implemented quickly and the nature of changes implemented varied considerably from one place to another arguably as a result of the Unit, District, and Regional health care organisations and authorities interpreting the recommendations in different ways. One striking change which was put in place by some organisations, for example, was to bring in personnel from non-healthcare backgrounds to manage services as general managers such as officers from the Armed Forces, business, and industry, for example.
The argument for Appropriate Physiotherapy Management and Leadership
On publication and Government acceptance of the Griffiths recommendations in 1984, the Council of the CSP set up a small working party under the Chairmanship of the author to formulate the Society’s policy and develop its response to the detrimental effects that the Griffiths changes were beginning to have on the leadership and management of physiotherapy services, the serious adverse consequences for provision of patient care and many important facets of the whole profession across the UK.
The membership of the working party was:
Robert Jones (Chairman), Bill Gilchrist (Member of Council, Chairman of the Industrial Relations Committee), Penelope Robinson (Director of Professional Affairs), Victoria Cichy (Director of Communications and Public Relations), Joyce Williams (Chair of Council (ex-officio), Philip Gray (Senior Industrial Relations Officer)
The group developed and set out guidance in the form of a “Briefing Paper” (below) which was widely used throughout physiotherapy and the NHS. Elements of the document were also picked up and used by other health professions. The Briefing Paper, “District Physiotherapy Management – why it must stay” sets out strong and clear arguments about what was considered to be the most appropriate management and leadership arrangements for physiotherapy services at all NHS levels in the UK. The paper was adopted by the CSP Council and provided a strong and successful basis for negotiating what was widely acknowledged within physiotherapy, by other professions and NHS employing authorities as providing an appropriate structure for the management, leadership, and provision of physiotherapy services. The author reported in his book “Management in Physiotherapy” (Radcliffe Medical Press Ltd, Oxford. 1991) that by 1989, 90% of all District Health authorities in England and Wales employed physiotherapists as District Physiotherapy Managers. It is clear that “District Physiotherapy Management – why it must stay” was a powerful and important primary source document.
Chartered Society of Physiotherapy
BRIEFING PAPER NO. 3 – December, 1984
DISTRICT PHYSIOTHERAPY MANAGEMENT
-WHY IT MUST STAY
In July 1984 the Government issued a Health Circular (84)13 entitled “Implementation of the NHS Management Inquiry (Griffiths) Report”. This calls for the appointment of the new General Managers at regional, district and unit levels throughout the NHS, but leaves the remainder of the management structure to be decided by the health authorities. This Circular is being rapidly implemented.
The Chartered Society of Physiotherapy is becoming concerned that some health authorities are misinterpreting the Health Circular by suggesting that district management of physiotherapy services should be abolished. This would not only return them to the discredited inefficient system of uncoordinated units which existed previously but would be a major step backwards for patient care, and contrary to the spirit of the Griffiths Report.
The profession of physiotherapy and the high standard of patient care which it provides is at an important crossroad. District physiotherapy management can work within the Griffiths general management system, provided that this system takes account of the needs of the profession related to the patients it serves. The Chartered Society of Physiotherapy believes that it would be a tragedy if the effective organisation and delivery of the physiotherapy service to the whole community is damaged purely for lack of information. This paper is therefore an attempt to ensure that health authorities and others are aware of the vital part that district physiotherapy management has to play now, and in the future.
The physiotherapy profession
Physiotherapy is the third largest direct patient care profession in the National Health Service next to nurses and doctors. It is an independent clinical profession which has expanded and developed significantly over the last ten years.
Physiotherapists assess, deal with and prevent problems of mobility and function using natural approaches based essentially on movement, manual therapy, and physical agencies. Physiotherapy has the primary aim of preventing injury, restoring or improving physical function and teaching self-care, to enable patient to lead as full and active a life as possible.
Physiotherapy remains a scarce resource in the health service and is much in demand: There is a national shortage of physiotherapists. Very few districts have more than 120 physiotherapy staff – the national average is only 15.2 per 100,000 population – and it is essential that these limited resources in any one district are carefully planned and managed across unit boundaries to ensure that the most effective patient care is provided.
The history of district physiotherapy management
The district physiotherapy manager is a recent innovation in the health service. Health authorities have acknowledged the advantages of these posts by rapid expansion of appointments in recent years, and to date over 180 health di9stricts have district physiotherapy management.
There is clear evidence that the appointments of managerial district physiotherapists has in most districts improved patient care within the community as a whole. This has been achieved by:
-
A more even distribution of scarce resources throughout a district;
-
The prevention of wasteful fragmentation and unnecessary duplication of expensive equipment between units;
-
Expansion of the service in Government priority areas such as community care;
-
Rotation of staff to ensure a service in the less popular units or “Cinderella” services such as care of the elderly, mentally ill or mentally handicapped. This is turn has helped recruit staff and improve morale.
In addition district physiotherapy managers have been able to assess and improve training facilities for staff within the district and provide specialist management expertise to the District Management Team.
The Chartered Society of Physiotherapy is committed to the retention and expansion of district physiotherapy management in England and Wales, together with area posts in Scotland and Northern Ireland. It strongly believes that the achievement of recent years should be build upon. It would be nonsensical if that achievement were destroyed in a mistaken attempt to fit physiotherapy services into rigid and inappropriate administrative models. The Griffiths Report itself contains a warning against just this kind of action: “there is a danger of over-organisation, of letting the machine designed to ensure a better service itself stifle the chances of getting one”.
Why district physiotherapy management must stay
If district physiotherapy management posts in their present form were not retained, the effective, economical and efficient provision of hight standards of patient care would be damaged. Physiotherapy is a cross-medical speciality and a cross-unit service. If cross-boundary physiotherapy services are impeded or made impossible – as they will be if district physiotherapy management is removed – then patient care will be the victim.
Physiotherapists deal with the patient’s functional problems after a medical diagnosis has been made, and the physiotherapy service has to follow the patient in a way in which virtually no other professional group in the NHS does. For example, an elderly patient with a circulatory disorder is admitted to an acute general unit and has an amputation. He is treated by a physiotherapist there, then passed on to the physiotherapy team rehabilitation unit, then on to the limb fitting centre. Finally, he will go either to the day hospital physiotherapist; to the community physiotherapist if he returns home; or receive physiotherapy in a residential home. He will pass through the hands of at least three separate teams of doctors and nurses. But for effective results, he has to be dealt with by a comprehensive physiotherapy service which operates across all these boundaries as an integrated team, and which can rapidly re-deploy staff across the district to meet changes of workload and the patient’s need for particular knowledge and skills.
There is also a grave danger that the provision of physiotherapy care in less “popular” areas such as the care of the elderly or mentally ill could be curtailed. With a national shortage of physiotherapists, staff will choose posts in hospitals or districts where they can gain the widest range of experience or work in more popular areas. Currently the agreed rotation of staff throughout a district, managed by the district physiotherapist, means that staff gain expertise in less popular specialties or units. In some cases this experience encourages them to stay in an area which they would not previously have considered. In addition, urgently needed cover in different parts of the district for staff sickness or other absence can be provided quickly by the reorganisation of priorities. All this would be lost with the imposition of unit budgets.
Without district managers there would also be professional problems which in turn would affect patient care. Physiotherapy is an independent, clinical profession separate from medicine. While accepting the need for administrative accountability to more senior management, physiotherapists cannot accept professional accountability to general managers, doctors, or anyone other than a member of their own profession. This professional accountability cannot be divorced from the control of the resources used to achieve the effective treatment of patients.
Districts physiotherapists effectively bridge the gap between professional and financial demands. Without them, future planning, and the rational expansion of physiotherapy services to fill priority gaps in services to patients within a district, could be replaced by unplanned and uneven development depending on which units put up the strongest arguments rather than patient needs across the district. This applies equally to the provision of expensive equipment, and co-ordinated professional training to meet district-wide needs.
District physiotherapy management has proved its worth in terms of economy and efficiency within the National Health Service, and this has been accepted by the great majority of district health authorities. It would be a tragedy for patient care if this gain were lost purely in the mistaken belief that Griffiths means the abolition of district physiotherapy manager posts. It does not. District physiotherapists are permitted under HC(84)13 which states that each health authority will have the maximum flexibility to make their own management arrangements, and that authorities should “have adequate scope to take due account of local management needs and potential”. The original Circular HC(79)19 which introduced the post of district physiotherapist into the health service remains in existence.
The way forward is to encourage the extension of district physiotherapy managers under the new general management arrangements, so that the physiotherapy profession can play its part in making Griffiths work. The Chartered Society of Physiotherapy is confident that, when they have reviewed the facts, health authorities will agree.
References:
CSP. 1984. Briefing Paper no.3 “District Physiotherapy Management – why it must stay”. CSP: London.
Jones RJ. 1991. Management in Physiotherapy, Radcliffe Medical Press Ltd: Oxford.
Jones RJ. 1987. The Development of Physiotherapy Management in the NHS in CSP Source Book, Parke Sutton Publishing: Norwich.
Jones RJ & Jenkins FC. 2006. Managing and Leading in the Allied Health Professions – Essential Guides. Radcliffe Publishing Ltd: Oxford.