Introduction¹
 My previous contribution to IPHA articles (March 2020) presented an overview of the relationship between the medical profession and physiotherapy following the introduction of the National Health Service (NHS) in the UK exemplified through the Cope Report. This contribution continues the story via an overview of the development of Registration and regulation of physiotherapy in the UK between the mid-1950s and early 21st century.
My previous contribution to IPHA articles (March 2020) presented an overview of the relationship between the medical profession and physiotherapy following the introduction of the National Health Service (NHS) in the UK exemplified through the Cope Report. This contribution continues the story via an overview of the development of Registration and regulation of physiotherapy in the UK between the mid-1950s and early 21st century.
Autonomy is an integral part of what it is to be a profession and the development of State Registration and later the evolution of Professional Regulation are crucial elements of autonomy which itself has many traits, for example, clinical practice, educational arrangements, management and leadership.
As a result of physiotherapy and the other professional groups refusing to co-operate with the tenor and recommendations of the Report (RJJ Article 1, 2020), the Cope Committee Report was abandoned by the Government despite pressure from the medical profession for implementation. Ian Macleod (the then Minister for Health) was unable to bring a Bill to the House of Commons to legislate on the Cope Committee recommendations as there was “insufficient agreement on fundamental matters” to proceed; (“Radiography”, 1953, P270). In view of this, the Minister recognised the credentials issued by the Professional Associations themselves as qualifications for employment in the NHS as a temporary measure. The Cope Report had provided clear evidence about the attitudes of the medical profession and the Ministry of Health officials towards the occupational groups concerned. The resistance to the Cope Report recommendations by the so-called “medical auxiliaries” (including physiotherapy) and the resulting abandonment of legislation by the Minister signified an important first step toward a negotiated level of autonomy for physiotherapy and the other occupational groups. However, medical control was to remain a powerful influence for some time to come as the Piercy Report (DHSS 1956) shows. This report set up by the Department of Health and Social Security under the Chairmanship of Lord Piercy stated: “within the NHS, physiotherapy is available only through the hospital service on the prescription and under the supervision of a specialist (doctor) since it is held that only in this way can it be given effectively and economically”. It had not been the remit of the Committee of Inquiry to report on “Medical Auxiliaries”, however, this statement shows that physiotherapy remained substantially under the control and direction of the medical profession.
Towards State Registration
The Minister of Health opened a discussion with the “Medical Auxiliaries” in 1954. For the first time, each of the professions involved was invited to nominate two delegates to the discussions which would encompass the possibility of a method of State Registration. The medical profession was not invited to send delegates to these negotiations, a totally new approach, in contrast to the tradition by which the Ministry of Health had always depended on the advice of doctors in any discussions about the future of these occupational groups. After several years of debate and discussion, the Professions Supplementary to Medicine Bill was introduced into the House of Commons in 1959, leading to the 1960 Act of Parliament; the proposed Legislation was strongly welcomed by the CSP. However, the British Medical Association (BMA) was opposed to the Professions Supplementary to Medicine Act, and the British Medical Journal represented the provisions of the Act as a defeat for the Medical Profession: “The composition of the Boards and Council proposed in the Bill shows that the medical view has not been conceded….the medical profession is right to claim that the professions supplementary to it should remain under its wing because the ultimate responsibility for treatment must lie with the doctor (BMJ 1959, P1164).
The PSM Act provided for the Registration of up to twelve occupational groups, initially, seven were involved: physiotherapists, dieticians, chiropodists, occupational therapists, medical laboratory technicians, radiographers, and remedial gymnasts; they had won the status of Professions Supplementary to Medicine which provided a statutory framework that allowed for them to have a degree of self-regulation, “to regulate themselves for the protection of their patients” (BMJ, vol. 284. P680, 1962). Other provisions of the Legislation in the CPSM Act 1960 included the executive capacity of the CSP in setting, conducting, and awarding its own qualification, requiring that all qualified physiotherapists should be State Registered to work within the NHS. The term “Professions Supplementary to Medicine replaced the previously used terms of “medical auxiliaries” and “paramedical”. The Statutory Registration system “adds not only this element of status, conditioning as it does both relations with other professions as well as relations with patients or clients who are served by the professions supplementary to medicine, it also carries with it connotations of proper qualifications and proper conduct” (Finch, J.D. 1984). For the first time, the word “Profession” was included in an official Government Act of Parliament with regard to physiotherapy and the other occupational groups involved, indicating official and public recognition of physiotherapy as a profession.
Under the provisions of the 1960 Act, the rules of the Physiotherapists’ Board stated: “no physiotherapist should treat a patient unless that patient has been referred to him/her by a Registered medical or dental practitioner, except in an emergency or some other exceptional reason, or unless he/she has direct access to the patient’s doctor (ibid).
Under the provisions of the Act of Parliament, each of the member professions of the CPSM was represented by a Board on the Council for Professions Supplementary to Medicine. The Physiotherapists’ Board comprised nine elected physiotherapists, six physicians, one educationalist and one physicist; the physiotherapy members, therefore, had a very slender majority on their own Board. However, all decisions of the Physiotherapists’ Board were referred to the Council for ratification and at this level, the physiotherapy curriculum was lost from total control by physiotherapists. The CPSM had 21 members, the Chairman of the Board, Sir Sydney Littlewood, a past President of The Law Society, together with representatives of the Privy Council and the DHSS. There were three medical representatives from the English colleges, two doctors representing the Scottish corporations and one representative of the General Medical Council. When all seats which could be occupied by doctors were so occupied, there would be eight of them. This would be a majority as the seven professions themselves were represented on the Council only by one member each, thus only one physiotherapist. The remaining seats were occupied by Civil Service appointees. The Registrar was a solicitor Mr J.S. Tapsfield and the first physiotherapist representative was Mr J.O. Jenkins who was chairman of the physiotherapists’ Board. Registration began in October 1962 and the first annual register was published in March 1963. The cost of registration was £5.00 with an annual retention fee of £2 10 shillings. State Registration was made compulsory in October 1964 and there were 8,800 physiotherapists on the register at that time. Prior to 1964, state registration was voluntary.
The CPSM was not the end of the decision-making process but was part of a larger hierarchy. Decisions ratified by the CPSM could be submitted to the Privy Council and thence to the Secretary of State in whom ultimate control was invested.
Implicit in State Registration, brought about by the setting up of the CPSM, was the increasing public recognition of physiotherapy; public confidence rests upon the knowledge of maintained standards. It was the responsibility of CPSM to regularly inspect schools of physiotherapy and they had the power to enforce changes recommended. Furthermore, any physiotherapist working in the NHS had to be registered with the CPSM and have undertaken training validated by CPSM.
From the CPSM to the development of the Health Professions Council (HPC)
Throughout the forty years between the introduction of physiotherapy State Registration in 1960 and the “winding up” of CPSM and introduction of the Health Professions Council (HPC) in 2000/2001many very significant and radical changes took place in society as a whole. There was much that would have important bearings on change and development in physiotherapy, for example: physiotherapy practice, professionalisation or possibly de-professionalisation, management and leadership, education, regulation, autonomy, innovation, to say nothing of changes in science and technology, politics, economics, population and demographics – the list goes on. The history of some of these issues as they affect physiotherapy such as autonomy, management and leadership and professionalisation/de-professionalisation will be subjects for some of my future contribution to IPHA articles. By the millennium the need for greatly strengthened Regulation had become necessary in many professions including physiotherapy and in many aspects of service provision and walks of life generally.
In the year 2000, the process of “winding up” the Council for Professions Supplementary to Medicine was underway.
I served for the last five years of the CPSM on the Physiotherapists’ Board, including membership of the Registration Committee and chairmanship of the Investigatory Committee.
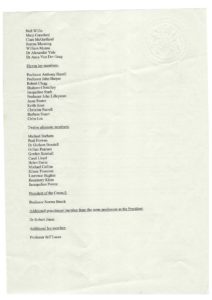
The document below, which is a letter of thanks from the President and Chief Executive Officer of the successor body for Regulation and Registration, the Health Professions Council was sent to all members of the CPSM following its final “winding up” at the end of the “Shadow” first year of the HPC. The CPSM had ceased functioning the year before when the Shadow new HPC came into place.

Following the repeal of the 1960 Professions Supplementary to Medicine Act a new Regulatory body – The Health Professions Council, (HPC) was established by means of the Health Professions Order 2001. It is interesting to note that the HPC was not set up by Act of Parliament, but just through the use of Parliamentary Statutory Instruments not requiring the introduction of a specific Bill into Parliament, secondary rather than primary legislation. The HPC started its preliminary activities in 2001 as a shadow organisation to undertake preliminary work in the development of the HPC while the CPSM continued regulatory activities until the Orders in Council received Royal Assent in 2002 when its powers ended and HPC came fully into being.
The HPC was an independent UK-wide Regulator of health professionals. It was set up to work on the basis of statutory self-regulation with accountability to the public, its Registrants, the Government (via the Privy Council) to whom it reported and to a range of other key stakeholders, for example, professional bodies, education providers and employers. The HPC was not part of the NHS or the Department of Health. Many of the Registrants were employed in the independent sector. The HPC was self-financing (registration fees being paid by the Registrants) it was a corporate body and as such, corporate governance was an important priority. The rules of the HPC were prepared during 2002/3 and finally approved by the Government in 2003.
The structure of the HHPC involved the Council and four Statutory committees: investigating, conduct and competence, health, and education and training. There was also a range of other sub-committees and panels. The membership of the Council comprised both Registrant members and lay members. The Legislation required that the registrant membership of the Council should exceed the lay membership by one seat. The lay members came with expertise from a wide range of backgrounds and were appointed through the Office of Public Appointments process by the Privy Council. Registrant members of the Council (one from each profession) were to be elected by their relevant profession and each Registrant had an alternate member to attend in the Registrant’s absence; the alternates were also nationally elected. In order to ensure full UK representation on the Council, it was a requirement that there must be at least one member from each of the four countries of the UK. The Council was led by a President (nominated by the Privy Council for the first appointment, but for subsequent appointments would be elected by the Council). The first President (Norma Brook) was an educator from physiotherapy, but Norma did not act in the capacity of a physiotherapist and was not in place to represent the physiotherapy profession, there was a physiotherapy Registrant on the Council nominated through the Privy Council, (myself!).
When the HPC was established there were twelve professions in membership:
- Art Therapists,
- Biomedical Scientists,
- Chiropodists and Podiatrists
- Clinical Scientists
- Dietitians
- Occupational Therapists
- Operation Department Practitioners
- Orthoptists
- Physiotherapists
- Prosthetists and Orthotists
- Radiographers
- Speech and Language Therapists
The purpose of the HPC was public protection primarily through the key processes of:
- Approval of programmes of education and training for entry to the Register
- Establishing and operating a Register
- Setting standards
- Intervening where a Registrants fitness to practice was alleged to be below standard.
Note: The document below is a reproduction of the Order of Appointment to the Health Professions Council which may be of interest as an original source. As can been seen, Norma Brook is listed as the President (nominated via the Privy Council; although a physiotherapist by background Norma’s position on the Council was required to be neutral, (not representing physiotherapy), hence my own appointment as the physiotherapy registrant member.
Over recent years, further changes have taken place in and to the registration and regulation body and process such as an increase in the number of professions regulated, the inclusion of social workers and changes to the membership of the Council in terms of how the professions are regulated for example. In line with changes that had taken place in the last decade the HPC has had a name change to the Health and Care Professions Council (HCPC) which reflects the many developments – however, that’s another story.
Clearly, physiotherapy registration and regulation has come a very long way since the 1950s, very significant changes which have contributed essential elements to the development of physiotherapy as a profession and development of professional autonomy together with the essential purpose of public protection. Registration and regulation arrangements in the UK have provided a template and basis for the development of many mechanisms in other countries around the world for the development of their own mechanisms and arrangements.
References are available for this material on request.
¹ As a nationally elected member of the Physiotherapists’ Board of the Council for Professions Supplementary to Medicine and later as the first physiotherapy member of the Health Professions Council, having been appointed by the Secretary of State and Privy Council, I recall much about the processes and politics around the development of professional regulation for physiotherapy in the UK. I have also researched this in-depth, particularly in the context of professionalisation, the development of autonomy – in all its aspects- and management and leadership of the profession.